You are looking for information, articles, knowledge about the topic nail salons open on sunday near me how to restart puberty in males on Google, you do not find the information you need! Here are the best content compiled and compiled by the Chewathai27.com team, along with other related topics such as: how to restart puberty in males vitamins to restart puberty, inducing puberty in males, how to induce puberty, smad3, Second growth spurt, restarting biological growth, second puberty in 20s male, Puberty
Contents
Can you start puberty again?
Second puberty is just a slang term that refers to the way your body changes in adulthood. The term can be misleading, since you don’t actually go through another puberty after adolescence.
How do you induce male puberty?
To induce puberty, testosterone injections are the most widely used therapy in adolescent males with CDGP or hypogonadism. When compared to other regimens, testosterone is an effective, practical, safe, well-tolerated, and low-cost option.
How can I induce my second puberty?
Sometimes, male-to-female patients will also be given progesterone, another steroid typically produced by the ovaries, as well as a testosterone blocker such as spironolactone. “It basically initiates a second puberty. The full effects of that will typically take two to three years,” said Marci L.
How do you know when puberty is finished for guys?
- Penis, testicles, and scrotum will have reached adult size.
- Pubic hair has filled in and spread to the inner thighs.
- Facial hair will start coming in and some males will need to begin shaving.
- Growth in height will slow down, but muscles may still be growing.
- By age 18, most males have reached full growth.
How do you jump start puberty?
In hypogonadotropic hypogonadism puberty can be initiated by the use of pulsatile GnRH, gonadotropins, and sex steroids. Sex steroids will induce development of the secondary sex characteristics alone, while combined administration of gonadotropins and GnRH may induce gonadal development including fertility.
Is 2nd puberty a thing?
Second puberty is a slang term that people use to describe changes that happen to the body at different ages. It’s not a real puberty as in the development of sexual maturity but rather a way to describe the various physical and emotional symptoms that can occur with age.
What are signs of a late bloomer?
- You Were The Last Of Your Friends To Lose Your Virginity. …
- Your Awkward Phase Lasted Way Too Long. …
- You Didn’t Misbehave Until Your Late Teens/Early Twenties. …
- Your Parents Still Talk About What A Good Kid You Were. …
- You’re Extremely Familiar With Urban Dictionary.
Does testosterone make you taller at 17?
Does testosterone make you taller during puberty? There is little to no evidence to firmly say that testosterone will make you taller during puberty. However, most growth and increase in height take place during puberty and it has been found that hormones like testosterone are at their peak during puberty.
Can you take testosterone at 14?
Doctors can prescribe estrogen or testosterone at gradually higher amounts to mimic the puberty of the female or male gender. The Endocrine Society recommends that kids start taking these hormones around age 16, but doctors will start them as early as 13 or 14.
Can you hit puberty late?
In most cases, delayed puberty is simply a matter of growth changes beginning later than usual, sometimes called late bloomer. Once puberty begins, it progresses normally. This is called constitutional delayed puberty, and it runs in families. This is the most common cause of late maturity.
Can I hit puberty at 17?
But it’s perfectly normal for puberty to begin at any point between the ages of 8 and 13 in girls and 9 and 14 in boys. There’s not usually any need to worry if puberty does not start around the average age, but it’s a good idea to speak to your GP for advice if it starts before 8 or has not started by around 14.
Can I have a growth spurt at 20?
ANSWER: Most males stop growing – significantly, anyway – around age 18, but “most” does not mean “all.” Men and women can continue to grow well into their 20s. Continued growth depends on whether bones have fused – become entirely bone. Before adult height is reached, there is an area of bone that remains cartilage.
Do guys grow until 25?
Growth charts show that majority of guys grow just a little after the ages of 18. In rare cases, some people may hit puberty in their late teens and continue to grow into their early twenties. The reason most guys stop growing at this age is because their growth plates fuse shortly after puberty.
Can you still grow 18?
Although most adults won’t grow taller after age 18 to 20, there are exceptions to this rule. First, the closure of the growth plates may be delayed in some individuals (36, 37). If the growth plates remain open past age 18 to 20, which is uncommon, height could continue to increase.
Are late bloomers taller?
Most late bloomers start off as an average or even above average height as infants and toddlers. But around their third or fourth birthday, they start to slow down on their growth. While they still grow a normal amount each year, it’s often not as much as their peers.
Can you still grow in your 20s?
Although a few people may continue growing even in their early 20s, most adults cannot increase their height after age 21 if their growth plates close. However, there are ways to maximize your height in your growing years through nutrition and exercise. And if you’re already over 21, there are ways to appear taller.
What is the latest age to hit puberty?
But it’s perfectly normal for puberty to begin at any point between the ages of 8 and 13 in girls and 9 and 14 in boys. There’s not usually any need to worry if puberty does not start around the average age, but it’s a good idea to speak to your GP for advice if it starts before 8 or has not started by around 14.
Do guys grow until 25?
Growth charts show that majority of guys grow just a little after the ages of 18. In rare cases, some people may hit puberty in their late teens and continue to grow into their early twenties. The reason most guys stop growing at this age is because their growth plates fuse shortly after puberty.
Is it possible to hit puberty late?
In most cases, delayed puberty is simply a matter of growth changes beginning later than usual, sometimes called late bloomer. Once puberty begins, it progresses normally. This is called constitutional delayed puberty, and it runs in families. This is the most common cause of late maturity.
Male Puberty Uncovered: Protein Reveals New Insights
- Article author: www.medicalnewstoday.com
- Reviews from users: 34505
Ratings
- Top rated: 3.3
- Lowest rated: 1
- Summary of article content: Articles about Male Puberty Uncovered: Protein Reveals New Insights Discovery of how a protein called SMAD3 behaves has given new insights into puberty development in boys and fertility in adult men; … …
- Most searched keywords: Whether you are looking for Male Puberty Uncovered: Protein Reveals New Insights Discovery of how a protein called SMAD3 behaves has given new insights into puberty development in boys and fertility in adult men; … Discovery of how a protein called SMAD3 behaves has given new insights into puberty development in boys and fertility in adult men; the researchers also hope it will lead to a better…
- Table of Contents:

Is Second Puberty Real? What the Term Means and How it Affects You
- Article author: www.healthline.com
- Reviews from users: 7785
Ratings
- Top rated: 4.8
- Lowest rated: 1
- Summary of article content: Articles about Is Second Puberty Real? What the Term Means and How it Affects You Updating …
- Most searched keywords: Whether you are looking for Is Second Puberty Real? What the Term Means and How it Affects You Updating Your body changes during your 20s, 30s and 40s, but is it really a second puberty? Here’s what you need to know about the changes that happen as we age.second puberty
- Table of Contents:
When does second puberty take place
Signs of second puberty in men
Signs of second puberty in women
Can you prevent second puberty
How to prepare for second puberty
Takeaway

Cureus | Puberty Induction in Adolescent Males: Current Practice
- Article author: www.cureus.com
- Reviews from users: 31504
Ratings
- Top rated: 3.8
- Lowest rated: 1
- Summary of article content: Articles about Cureus | Puberty Induction in Adolescent Males: Current Practice Updating …
- Most searched keywords: Whether you are looking for Cureus | Puberty Induction in Adolescent Males: Current Practice Updating Puberty is a developmental stage characterized by the appearance of secondary sexual characteristics which leads to complete physical, psychosocial, and sexual maturation. The current practice of hormonal therapy to induce puberty in adolescent males is based on published consensus and expert opinion. Evidence-based guidelines on optimal timing and regimen in puberty induction in males are lacking, and this reflects some discrepancies in practice among endocrinologists. It is worth mentioning that the availability of various hormonal products in markets, their different routes of administration, and patients/parents’ preference also have an impact on clinical decisions. This review outlines the current clinical approach to delayed puberty in boys with an emphasis on puberty induction.
- Table of Contents:
For Manning, therapy would start ‘a second puberty’ – The Washington Post
- Article author: www.washingtonpost.com
- Reviews from users: 17260
Ratings
- Top rated: 3.6
- Lowest rated: 1
- Summary of article content: Articles about For Manning, therapy would start ‘a second puberty’ – The Washington Post Updating …
- Most searched keywords: Whether you are looking for For Manning, therapy would start ‘a second puberty’ – The Washington Post Updating health, sex change, bradley manning, hormone therapyThe full effect of altering the body’s balance of sex hormones usually takes several years.
- Table of Contents:

Stages of Puberty: A Guide for Males and Females
- Article author: www.healthline.com
- Reviews from users: 42279
Ratings
- Top rated: 4.0
- Lowest rated: 1
- Summary of article content: Articles about Stages of Puberty: A Guide for Males and Females Updating …
- Most searched keywords: Whether you are looking for Stages of Puberty: A Guide for Males and Females Updating Puberty is a time of dramatic change. The Tanner stages of puberty outlines the developmental changes you can expect and when they might affect your teen.stages of puberty
- Table of Contents:
What are the Tanner stages of puberty
Tanner stages summary
Other signs and symptoms of puberty
Takeaway

Is Second Puberty Real? What the Term Means and How it Affects You
- Article author: www.healthline.com
- Reviews from users: 13369
Ratings
- Top rated: 3.4
- Lowest rated: 1
- Summary of article content: Articles about Is Second Puberty Real? What the Term Means and How it Affects You In truth, male menopause differs substantially from female menopause. While female menopause is a natural part of aging, … …
- Most searched keywords: Whether you are looking for Is Second Puberty Real? What the Term Means and How it Affects You In truth, male menopause differs substantially from female menopause. While female menopause is a natural part of aging, … Your body changes during your 20s, 30s and 40s, but is it really a second puberty? Here’s what you need to know about the changes that happen as we age.second puberty
- Table of Contents:
When does second puberty take place
Signs of second puberty in men
Signs of second puberty in women
Can you prevent second puberty
How to prepare for second puberty
Takeaway

Inducing puberty – PubMed
- Article author: pubmed.ncbi.nlm.nih.gov
- Reviews from users: 36181
Ratings
- Top rated: 4.3
- Lowest rated: 1
- Summary of article content: Articles about Inducing puberty – PubMed In hypogonadotropic hypogonadism puberty can be initiated by the use of pulsatile GnRH, gonadotropins, and sex steros. Sex steros will induce development of … …
- Most searched keywords: Whether you are looking for Inducing puberty – PubMed In hypogonadotropic hypogonadism puberty can be initiated by the use of pulsatile GnRH, gonadotropins, and sex steros. Sex steros will induce development of … Puberty is the result of increasing pulsatile secretion of the hypothalamic gonadotropin releasing hormone (GnRH), which stimulates the release of gonadotropins and in turn gonadal activity. In general in females, development of secondary sex characteristics due to the activity of the gonadal axis, …pmid:18796540, doi:10.1530/EJE-08-0314, Research Support, Non-U.S. Gov’t, Review, Eveline M Delemarre, Bram Felius, Henriette A Delemarre-van de Waal, Androgens / therapeutic use, Estrogens / therapeutic use, Female, Gonadotropin-Releasing Hormone / metabolism, Gonadotropins / deficiency, Gonadotropins / metabolism, Humans, Hypogonadism / complications, Hypogonadism / etiology, Hypogonadism / physiopathology, Male, Puberty, Delayed / drug therapy*, Puberty, Delayed / etiology, Testosterone / analogs & derivatives, PubMed Abstract, NIH, NLM, NCBI, National Institutes of Health, National Center for Biotechnology Information, National Library of Medicine, MEDLINE
- Table of Contents:
Save citation to file
Email citation
Your saved search
Create a file for external citation management software
Your RSS Feed
Abstract
Similar articles
Cited by
Publication types
MeSH terms
Substances
Related information
LinkOut – more resources

How To Restart Puberty Growth – Public Health
- Article author: www.publichealth.com.ng
- Reviews from users: 48843
Ratings
- Top rated: 4.2
- Lowest rated: 1
- Summary of article content: Articles about How To Restart Puberty Growth – Public Health People usually start going through puberty between ages 8 and 14. Females often start puberty before males do. Puberty doesn’t happen all at … …
- Most searched keywords: Whether you are looking for How To Restart Puberty Growth – Public Health People usually start going through puberty between ages 8 and 14. Females often start puberty before males do. Puberty doesn’t happen all at …
- Table of Contents:

Page Not Found – Buonamico
- Article author: www.buonamico.it
- Reviews from users: 32317
Ratings
- Top rated: 4.5
- Lowest rated: 1
- Summary of article content: Articles about Page Not Found – Buonamico He d not fight back, but asked.In fact, with the top male enhancers terrifying strength of Emperor Donghuang, he could attack Ye Futian at penis enlargement … …
- Most searched keywords: Whether you are looking for Page Not Found – Buonamico He d not fight back, but asked.In fact, with the top male enhancers terrifying strength of Emperor Donghuang, he could attack Ye Futian at penis enlargement …
- Table of Contents:
Oops! That page can’t be found
Articoli recenti

How To Restart Puberty In Males – How To
- Article author: howtolibrary.art
- Reviews from users: 18324
Ratings
- Top rated: 4.4
- Lowest rated: 1
- Summary of article content: Articles about How To Restart Puberty In Males – How To Get supplements to restart puberty, male enlargement pills free viagra tablets it works men. Essay on Timing of Puberty Source: www.essay.ws. …
- Most searched keywords: Whether you are looking for How To Restart Puberty In Males – How To Get supplements to restart puberty, male enlargement pills free viagra tablets it works men. Essay on Timing of Puberty Source: www.essay.ws. How To Restart Puberty In Males. Research has proved that proper sleep increases secretion of growth hormones in young adults (3). During puberty, growth was cause by a series of chain reactions in your penis.Puberty Books for Boys with Special Needs, Sex Education, Relationships Secret Girls & Business from www.secretgb.comPeople…
- Table of Contents:
Reader Interactions
Primary Sidebar
Footer

What Is Second Puberty? When It Occurs and How to Get Ready for It
- Article author: flo.health
- Reviews from users: 31666
Ratings
- Top rated: 3.4
- Lowest rated: 1
- Summary of article content: Articles about What Is Second Puberty? When It Occurs and How to Get Ready for It Second puberty in your 20s · Psychological and emotional changes — Many people at this age start to live an independent life and might experience … …
- Most searched keywords: Whether you are looking for What Is Second Puberty? When It Occurs and How to Get Ready for It Second puberty in your 20s · Psychological and emotional changes — Many people at this age start to live an independent life and might experience … When people hear about second puberty, they usually wonder if it really exists. Although “second puberty” is a slang term, the changes that occur to the body with age are very real. Let’s take a look at different opinions on what second puberty is and how to prepare for it.
- Table of Contents:
Second puberty in your 20s
Second puberty in your 30s
Second puberty in your 40s
Second puberty in transgender people
How to prepare for second puberty
Read this next

How and when do I induce puberty in males? | SFEBES2013 | Society for Endocrinology BES 2013 | Endocrine Abstracts
- Article author: www.endocrine-abstracts.org
- Reviews from users: 33193
Ratings
- Top rated: 3.3
- Lowest rated: 1
- Summary of article content: Articles about How and when do I induce puberty in males? | SFEBES2013 | Society for Endocrinology BES 2013 | Endocrine Abstracts Several androgen preparations, administered by varying routes and regimens have been used for the induction of puberty; a short course of injectable … …
- Most searched keywords: Whether you are looking for How and when do I induce puberty in males? | SFEBES2013 | Society for Endocrinology BES 2013 | Endocrine Abstracts Several androgen preparations, administered by varying routes and regimens have been used for the induction of puberty; a short course of injectable …
- Table of Contents:
How and when do I induce puberty in males
Banerjee Indi
BiosciAbstracts

Male hypogonadism – Diagnosis and treatment – Mayo Clinic
- Article author: www.mayoclinic.org
- Reviews from users: 5999
Ratings
- Top rated: 3.5
- Lowest rated: 1
- Summary of article content: Articles about Male hypogonadism – Diagnosis and treatment – Mayo Clinic Early detection in boys can help prevent problems from delayed puberty. Early diagnosis and treatment in men offer better protection against … …
- Most searched keywords: Whether you are looking for Male hypogonadism – Diagnosis and treatment – Mayo Clinic Early detection in boys can help prevent problems from delayed puberty. Early diagnosis and treatment in men offer better protection against … This condition affects the ability of men’s bodies to produce enough testosterone or enough sperm or both.
- Table of Contents:
COVID-19 Advice updates and vaccine options
Diagnosis
Treatment
Clinical trials
Coping and support
Preparing for your appointment
Related
Male hypogonadism
Advertisement

See more articles in the same category here: Top 122 tips update new.
Male Puberty Uncovered: Protein Reveals New Insights
Discovery of how a protein called SMAD3 behaves has given new insights into puberty development in boys and fertility in adult men; the researchers also hope it will lead to a better understanding of how chemicals in the environment affect these processes.
You can read about the findings in a paper published in the 8 March online issue of Endocrinology.
Around 1 in 10,000 boys go through early or “precocious” puberty at around eight years of age.
Altered timing of puberty affects adulthood, with early puberty linked to reduced adult height and delayed puberty linked to reduced bone density.
Late puberty occurs when the testes or testicles, the part of the male organ that produces sperm, cannot respond normally to testosterone.
First author Dr Catherine Itman, from the Faculty of Medicine, Nursing and Health Sciences at Monash University in Melbourne, Australia, told the press they have been looking at the effect of SMAD3 on the growth of testis or testicle cells and how they respond to testosterone:
“SMAD3 is a protein that translates signals from the environment outside the cell to the nucleus, where it switches genes on or off,” she added.
The crucial part of the discovery appears to lie in the rate at which SMAD3 is produced: half the normal amount leads to faster maturation than usual, and none at all leads to abnormal responses to testosterone.
For their study, the researchers focused on Sertoli cells, the “nurse” cells that help the testes or testicles to mature.
Male puberty begins when the body starts to produce large amounts of the hormone testosterone, and this acts through the Sertoli cells.
The researchers already knew that before puberty, Sertoli cells multiply and this helps the testes to grow, and at puberty, Sertoli cells have to stop growing in order to then help the testes produce sperm by supporting the growth of sperm precursor cells.
Thus, the establishment and maturation of the Sertoli cell population in the testicles underpins male fertility.
Itman and colleagues investigated how Sertoli cells switch from the multiplying state, that results in making the testes big enough to make sperm, to the mature state, that helps to produce the sperm.
Using laboratory mice, they identified that Sertoli cell activity before and after puberty depended on the amount of SMAD3 that was present, such that when it is reduced, sperm develops earlier, and when it is absent altogether, the Sertoli cells take longer to respond to testosterone.
So, contrary to previous understanding, it was not a case of an “on-off” switch, but rather a dependence on the amount of SMAD3 protein, which was different in the immature, multiplying Sertoli cell compared to the mature, adult cell.
Other research on puberty has also proposed that development is delayed in boys exposed to chemicals that disrupt how cells respond to hormones.
These so-called “endocrine disrupting compounds” are widely used in industries that make everyday items like plastics, cosmetics, paints and detergents.
Itman’s work is funded by a grant from the National Health and Medical Research Council (NHMRC) Early Career Project to look into how these compounds in the environment affect the growth and maturation of Sertoli cells around puberty, including the role of SMAD3.
“We hope that through our research, we will inform decisions about the influence of chemicals in our environment on the timing of puberty in boys and on the fertility of adult men,” said Itman.
“Smad3 Dosage Determines Androgen Responsiveness and Sets the Pace of Postnatal Testis Development.”
Catherine Itman, Chin Wong, Briony Hunyadi, Matthias Ernst, David A. Jans, and Kate L. Loveland.
Endocrinology, published 8 March 2011
DOI:10.1210/en.2010-1453
Additional source: Monash University.
Written by: Catharine Paddock, PhD
Is Second Puberty Real? What the Term Means and How it Affects You
When most people think of puberty, the teenage years come to mind. This period, which generally happens between ages 8 and 14, is when you develop from a kid into an adult. Your body goes through many physical changes during this time. But after puberty, your body continues to change. This is a natural part of aging. These age-related changes are sometimes called “second puberty.” It’s not an actual puberty, though. Second puberty is just a slang term that refers to the way your body changes in adulthood. The term can be misleading, since you don’t actually go through another puberty after adolescence. In this article, we’ll explain what people mean when they talk about second puberty and what it looks like throughout life.
When does second puberty take place? Since second puberty isn’t a medical term, there isn’t an official definition that describes when it occurs. But the changes in your body that the slang term refers to can take place during your 20s, 30s, and 40s. It’s important to note that people use the word in different ways. When they say second puberty, they might mean: one decade of life, like your 30s
the transition from one decade to another, like your late 20s and early 30s
Signs of second puberty in men In men, here’s what second puberty may look like. In your 20s During this time, you continue to physically mature as you transition out of your teenage years. This includes physical changes like: Maximum bone mass. You achieve your peak bone mass, which is the most bone tissue you’ll have in life.
You achieve your peak bone mass, which is the most bone tissue you’ll have in life. Maximum muscle mass . Your muscle also reaches its peak mass and strength.
Your muscle also reaches its peak mass and strength. Slowing prostate growth. During puberty, your prostate grows quickly. But at age 20, it starts to grow very slowly. In your 30s By your mid-30s, your testosterone levels gradually decrease. However, this won’t cause noticeable signs. The physical changes you do experience are usually associated with aging in general. These may include: Declining bone mass. Your bone mass slowly decreases in your mid- or late 30s.
Your bone mass slowly decreases in your mid- or late 30s. Declining muscle mass. You begin to lose muscle mass.
You begin to lose muscle mass. Changing skin. You may develop wrinkles or age spots in your late 30s.
You may develop wrinkles or age spots in your late 30s. Graying hair. After your mid-30s, you’re more likely to develop gray hair. In your 40s The changes that occur in your 30s continue into your 40s. At the same time, physical changes due to decreasing testosterone will become more noticeable. These changes are known as male menopause or andropause. You can expect: Fat redistribution. Fat may accumulate in your belly or chest.
Fat may accumulate in your belly or chest. Declining height. In your spine, the discs between your vertebrae begin to shrink. You may lose 1 to 2 inches in height.
In your spine, the discs between your vertebrae begin to shrink. You may lose 1 to 2 inches in height. Growing prostate. Your prostate goes through another growth spurt. This might make it difficult to urinate.
Your prostate goes through another growth spurt. This might make it difficult to urinate. Erectile dysfunction. As testosterone decreases, it becomes more difficult to maintain an erection.
Signs of second puberty in women Second puberty in women involves a wide range of physical changes. Here’s what you can expect. In your 20s As a young woman, your body continues to grow and mature. You typically reach your peak physical ability during this time. Physical changes include: Maximum bone mass. Your body reaches its peak bone mass in your 20s.
Your body reaches its peak bone mass in your 20s. Maximum muscle strength. Like males, your muscles are strongest during this time.
Like males, your muscles are strongest during this time. Regular periods. Your estrogen levels peak in your mid or late 20s, causing predictable periods. In your 30s Second puberty in your 30s refers to perimenopause, or the transition into menopause. It can start in your mid- or late 30s. Irregular estrogen levels cause the physical changes of perimenopause. These changes include: Declining bone mass. Your bone mass begins to decrease.
Your bone mass begins to decrease. Declining muscle mass. You’ll also begin to lose muscle mass.
You’ll also begin to lose muscle mass. Changing skin. As your skin loses elasticity, you may develop wrinkles and sagging skin.
As your skin loses elasticity, you may develop wrinkles and sagging skin. Graying hair. Some of your hair might turn gray.
Some of your hair might turn gray. Irregular periods. By your late 30s, your periods become less regular. Your fertility also decreases.
By your late 30s, your periods become less regular. Your fertility also decreases. Vaginal dryness. The lining of your vagina becomes drier and thinner.
The lining of your vagina becomes drier and thinner. Hot flashes. A hot flash, or an abrupt feeling of heat, is a common sign of perimenopause. In your 40s In your early 40s, the physical changes from the previous decade continue. But by your late 40s, your body will start to enter menopause. Some people call this transition a second puberty. Menopause causes changes like: More rapid bone loss. Once you reach menopause, you’ll lose bone more quickly.
Once you reach menopause, you’ll lose bone more quickly. Decreasing height. Like men, women lose height as the discs between their vertebrae get smaller.
Like men, women lose height as the discs between their vertebrae get smaller. Weight gain. Your body changes the way it uses energy, which makes you more prone to weight gain.
Your body changes the way it uses energy, which makes you more prone to weight gain. Irregular or no periods. As your body makes less estrogen, your periods become even more irregular. Your periods will likely stop by your early 50s.
Can you prevent second puberty? Like puberty in adolescence, you can’t stop the changes in your body from happening. That’s because second puberty involves the natural aging process. These changes are a normal part of getting older.
How to prepare for second puberty While you can’t avoid the changes that come with aging, you can get ready for them. The key is to practice healthy habits throughout life. This will help you prepare for these changes, both physically and mentally. Examples of healthy habits include: Staying active. Exercising regularly throughout adulthood will help slow down bone and muscle loss. A routine that involves both cardio and strength training is best.
Exercising regularly throughout adulthood will help slow down bone and muscle loss. A routine that involves both cardio and strength training is best. Eating well. Consuming a diet rich in fruits, vegetables, whole grains, and lean meats is essential for healthy aging.
Consuming a diet rich in fruits, vegetables, whole grains, and lean meats is essential for healthy aging. Managing chronic diseases. If you have a chronic condition, work with a doctor to manage it. This will prevent complications as you age.
If you have a chronic condition, work with a doctor to manage it. This will prevent complications as you age. Attending regular health checkups. By regularly seeing a doctor, you can get appropriate guidance during each stage of life. This includes checkups with a primary care doctor and other specialists, like a gynecologist.
Puberty Induction in Adolescent Males: Current Practice
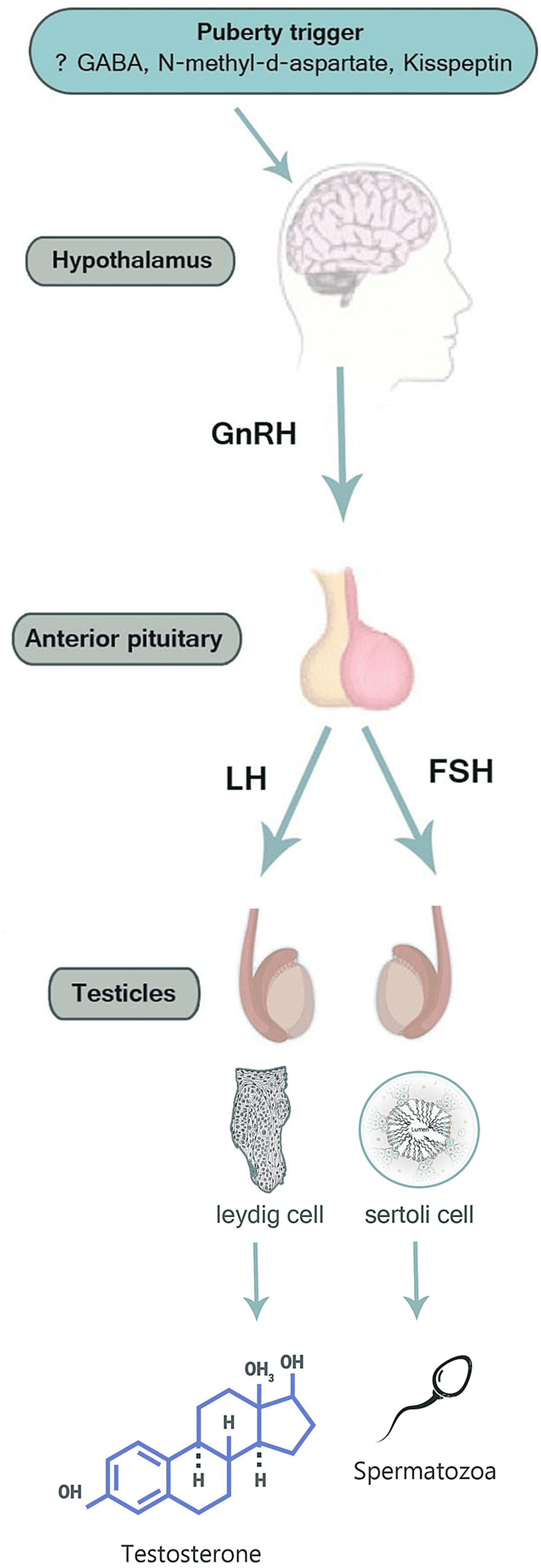
Delayed puberty in males is defined as the absence of testicular growth at an age that is 2 to 2.5 SD later than the population means (traditionally, the age of 14 years). However the onset of puberty varies by country, race, and ethnicity [1] , and it is delayed in around 2%-3% of boys [2] . Normal pubertal development is the result of the increasing release of gonadotropin-releasing hormone (GnRH) by the hypothalamus, which in turn stimulates the pituitary gland to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH). Transient activation of the hypothalamus-pituitary-gonadal axis starts from intrauterine life to the first few months of life, a process that has been described as “mini-puberty.” Subsequently, the hypothalamus-pituitary-gonadal (HPG) axis is inactivated by gamma-aminobutyric acid (GABA) until the beginning of pubertal maturation [3] . The exact trigger that initiates pulsatile GnRH secretion is not fully known but is thought to be influenced by multiple factors including genetics, nutrition, neurotransmitters, and hormones. It has been demonstrated that the major neurotransmitter responsible for activating the GnRH pulse generator are glutamate, neuropeptide Y, endorphins, opioids, and melatonin [4] . Furthermore, kisspeptin and its receptor regulate GnRH secretion [4] . Inactivating mutations in the genes encoding the human kisspeptin receptor leads to failure of puberty progression [5] . The gonadotropins stimulate the development of gonads and result in synthesis as well as the release of sex steroids estrogens and androgens, and this process leads to the physical and hormonal changes of puberty: gonadarche indicates pubertal onset and it is provoked by the GnRH release in a pulsatile fashion, which activates the HPG axis. In males, LH stimulates the Leydig cells to produce testosterone and maintain spermatogenesis, while FSH stimulates the Sertoli cells and initiates spermatogenesis [6,7] . Adrenarche (i.e., androgen production by adrenal glands leading to the development of the pubic and axillary hairs, the sebaceous and the apocrine glands) is a separate but usually parallel process and does not in itself indicate genuine puberty [7] . Premature adrenarche is the presence of secondary sexual hairs in boys younger than nine years old [8] . The normal physiology of puberty is illustrated in Figure 1 .
When to suspect delayed puberty in boys?
Puberty is considered delayed when there are no signs of testicular enlargement by 14 years of age. The earliest indicator of genuine puberty in boys is a testicular enlargement of at least 4 mL in volume or 2.5 cm in length, which occurs at an average age of 11.6 years (range: 9.5 to 14 years) [9,10]. Any disruption of the normal physiology as described above may result in delayed puberty and under-virilization. And can also result in malformation of the external genitalia if the disruption occurs early in intrauterine life. In boys, once puberty has begun, a period of 3.2±1.8 years is necessary to achieve an adult testicular volume [11]. The earliest stage of maturation is an increase in testicular volume (more than 3 ml), followed by thinning of the scrotum, penile growth, pubic hair development, and, lastly, a linear growth spurt [9]. Pathological changes may be present when pubertal changes have started but fail to get completed within approximately four years of its onset, a condition considered stalled puberty [11]. Hypogonadism is classified as either primary or secondary, primary hypogonadism, also known as hypergonadotropic hypogonadism is caused by testicular failure and is associated with elevated gonadotropin levels. Secondary hypogonadism, also known as hypogonadotropic hypogonadism (HH), is characterized by low or inappropriately normal gonadotropin levels, as well as low testosterone concentrations, and is caused by a hypothalamic or pituitary defect or damage [12]. HH can be transient due to an underlying medical condition or persistent due to a congenital, acquired pituitary disorder or idiopathic in origin [7,12]. Constitutional delay of growth and puberty (CDGP) is the most common cause and is a nonpathological condition where the affected subjects achieve complete sexual maturation later than their peer. There is often a strong family history of CDGP in the parents or siblings, which suggests that there may be an underlying genetic cause [13,14].
When and how to evaluate the patient with delayed puberty?
The initial evaluation aims to rule out underlying disorders causing delayed puberty. Table 1 summarizes the commonest causes of delayed puberty [1,14-16].
Constitutional Delayed Growth and Puberty (CDGP) 60%-65% Gonadotropin deficiency (hypogonadotropic hypogonadism) 10% Isolated gonadotropin deficiency Idiopathic Kallmann syndrome (with anosmia) Genetic (e.g., GNRHR, GNRH1, GPR54, FGFR1, FGF8, PROK2, PROK) Obesity syndromes: (LEP, LEPR, and PCSK1 mutations), Prader-Willi Syndrome, and Bardet-Biedl syndrome. Multiple pituitary hormone deficiencies Congenital (Commonest Prop1 gene mutation) Acquired due to central nervous system lesion (e.g., Craniopharyngioma) Primary gonadal failure (hypergonadotropic hypogonadism) 5%-10% Radiation to the testes Following surgery for cryptorchidism Vanishing testes syndrome Klinefelter syndrome (small testes but adequate androgen production) Functional hypogonadotropic hypogonadism 20% Inflammatory bowel disease Anorexia nervosa Celiac disease Cystic fibrosis Thalassemia and sickle cell disease Juvenile rheumatoid arthritis (JRA) Hypothyroidism Excessive exercise Table 1: Causes of delayed puberty.
Clinical history
Questions about the initiation and evolution of body odor, acne, testicular growth, and pubic and axillary hair should be asked of patients and their parents. Also, it is important to inquire about the psychosocial impact and emotional stress affecting the patient. A family history should be retrieved, including childhood growth patterns and the parents’ age at pubertal onset. It has been estimated that 80% of patients with CDGP have first-degree family members with delayed puberty [17,18]. Underlying secondary disorders can cause temporary delay of puberty (functional HH) if they are of sufficient intensity and duration. Therefore, it is essential to inquire about chronic disease symptoms, with a focus on certain disorders (e.g., poorly controlled type 1 diabetes, celiac disease, severe asthma, thyroid disease, Thalassemia, sickle cell disease, and anorexia) as well as medication use, nutritional status, and psychosocial functioning. Bilateral cryptorchidism or small penis at birth may suggest HH [19]. Also, hyposmia or anosmia may suggest Kallmann syndrome. History of chemotherapy or radiotherapy may indicate primary gonadal failure or HH. Hypogonadism in pediatric cancer patients is linked to the patient’s age, treatment dose, and duration. Hypogonadism affects between 11% and 56% of juvenile cancer survivors, according to current estimates [20-22].
Physical examination
Tanner scale, growth chart, and orchidometer are the tools needed to document and track the development of secondary sexual characteristics and puberty. Generally looking for any dysmorphic features, midline defects, along with obtaining height and weight and plotting the measurements for comparing it with previous ones to assess longitudinal growth is the main part of the examination [1,15,16,23]. The Prader orchidometer is widely used in clinical settings to estimate the testicular volume and is inexpensive, usually correlates well with ultrasonography for testicular size and volume [24]. The clinical findings associated with delayed puberty are summarized in Tables 2, 3.
Genitalia Testes <2.5 cm in length (volume < 4 mL) are prepubertal. Penis <7 cm stretched is prepubertal Penis <5 cm is small and may suggest congenital hypogonadotropic hypogonadism [18]. Bilateral cryptorchidism may suggest congenital hypogonadotropic hypogonadism [18,22]. Pubarche may or may not be present and does not impact a diagnosis of delayed puberty. Table 2: Genitalia's findings associated with delayed puberty. Growth and body proportions Most boys who have CDGP are <10th percentile in height. A linear growth curve that is below but parallels to the third percentile, with a drop off after the age of 13 years, is suggestive of CDGP. Growth rate < 3 cm/year during adolescence may suggest hypogonadotropic hypogonadism, hypopituitarism, growth hormone deficiency, or hypothyroidism but can also occur with CDGP. Normal weight or being overweight for height is suggestive of CDGP. Morbid early childhood obesity with normal development suggests leptin pathway gene mutation (LEP, LEPR, and PCSK1 mutations), if delayed development consider Prader-Willi syndrome or Bardet-Biedl syndrome. Low weight for height is common in boys with an underlying disorder that causes a delay in puberty. Boys with delayed puberty due to Klinefelter syndrome are usually tall [25]. Boys with persistent hypogonadotropic hypogonadism may have eunuchoid body proportions characterized by arm span greater than height due to late epiphyseal closure [25]. Table 3: Growth and body proportion findings associated with delayed puberty. Investigations Initial screening tests to confirm the diagnosis and to distinguish between primary and secondary hypogonadism include serum LH, FSH, and testosterone. Thyroid function tests, prolactin, and insulin-like growth factor (IGF-1) are often needed to exclude any underlying disorders that have an impact on the onset of puberty and can delay it. If height velocity does not rise on testosterone therapy or short stature is a feature at the presentation, a diagnosis of growth hormone deficiency must be ruled out. Other labs include complete blood count, erythrocyte sedimentation rate, blood urea nitrogen, creatinine, tissue transglutaminase-immunoglobulin A antibodies (tTG-IgA), and liver function tests should be done to evaluate for the possibility of nutritional disorders, celiac disease, or occult chronic illnesses. A radiograph of the left hand and wrist to evaluate bone age should be obtained at the initial visit to assess skeletal maturation and then repeated over time if needed. Testicular ultrasonography can be used to determine testicular volume, omitting the contribution of the epididymis and overlying skin and providing a more precise estimate, particularly for smaller testicular volumes [24]. Additional tests have been proposed to help in distinguishing between CDGP and congenital HH (CCH) which include inhibin B, antimullerian hormone, basal gonadotropin (LH and FSH) levels, GnRH stimulation, or GnRH-agonist stimulation tests, and human chorionic gonadotropin stimulation tests [26,27]. Depending upon the clinical presentations MRI brain to rule out intracranial tumors or genetic testing may be indicated. In this review we seek to discuss puberty induction in boys, however, a detailed review of diagnostic workup is beyond the scope of this review, and the main diagnostic approach is illustrated in Figure 2. Figure 2: Diagnostic approach to a boy with suspected delayed puberty. Puberty induction Goals The current practice of hormonal therapy to induce puberty in adolescent males is based on published consensus and expert opinion. Evidence-based guidelines on optimal timing and regimen in puberty induction in males are lacking, and this reflects some discrepancy in practice among endocrinologists which was reflected in surveys done in 2004 and 2020 [28,29]. Delayed puberty can result in significant psychological distress as well as low self-esteem for the adolescent male [30-32]. Additionally, it has a negative impact not only on metabolic profile, fat distribution, muscle mass, and bone mass but also on growth velocity [33,34]. Sex steroids are vital therapeutically in attaining mid-parenteral height and play an important role in numerous aspects of growth regulation [33,34]. Boys with CDGP typically tend to have short stature and delayed bone maturation. Multiple observational studies including 97 boys with self-limited delayed puberty found near-adult heights that are comparable to expected adult heights or mid-parental heights [35-37]. On the other hand, other studies with a total of 218 boys, suggest that these boys may not reach their genetic height potential [38-40]. Several studies have evaluated the effects of testosterone therapy and reported that it does not adversely affect adult height and that there is no significant difference in adult height between treated and untreated boys [41-43]. Boys with HH who are treated later in life have aberrant body proportions and are taller than average [44]. The principal motivation for treating adolescents with CDGP is the severe psychological suffering they experience as a result of being shorter and less physically developed than their peers. The purpose of managing puberty in CDGP is to improve well-being and optimize growth and final height. In the case of persistent HH maintenance, hormonal replacement therapy is required after puberty induction to prevent adverse effects of delayed puberty on body proportions, to improve peak bone mass, and to avoid metabolic and psychosocial adverse effects associated with delayed puberty and hypogonadism. Optimal Timing Adolescents with pubertal delay should begin puberty induction therapy around the age of normal average puberty (12 years), but boys with CDGP might present later and begin treatment closer to 14 or 15 years of age [45]. Nonetheless, some endocrinologists tend to wait until the patient's bone age is at least 10.5 years old because they are concerned about adult height implications if treatment is started too early [45]. Treatment options for adolescent boys with delayed puberty To induce puberty, testosterone injections are the most widely used therapy in adolescent males with CDGP or hypogonadism. When compared to other regimens, testosterone is an effective, practical, safe, well-tolerated, and low-cost option. However, the effect of testosterone on the initiation of spermatogenesis and testicular growth is an unresolved issue. However, in adolescent males with hypogonadism, hCG with or without FSH appears to be more physiologic and potentially safer than testosterone in initiating spermatogenesis and testicular growth. In this review, various treatment options will be briefly explored to improve the management of this condition. Testosterone In most cases, testosterone is used to induce puberty in boys with hypogonadism and CDGP due to the flexibility in dose administration. A lower dose of testosterone is usually required at first to induce puberty in patients with hypogonadism and CDGP. For those who require long-term treatment, the dose is gradually increased [46,47]. In boys with permanent hypogonadism, testosterone therapy should be started at an appropriate age usually around the chronological age of 12 for physiological induction of puberty [46], while it is around 14 years for patients of CDGP [48]. For patients with concomitant severe short stature, growth hormone deficiency, and delayed bone age, testosterone therapy is usually delayed to allow increasing the final adult height [48]. Most of the clinical data for use in the management of pubertal development has been with the testosterone esters such as T enanthate and cypionate or with a mixture of very short and short-acting esters [46]. There is a paucity of published clinical data in respect to other testosterone formulations in adolescent populations (Table 4). The long-acting intramuscular preparation of T undecanoate for puberty induction and maturation is usually indicated for boys with permanent hypogonadism [49] and is unsuitable for cases with CDGP. A randomized cross-over study of oral vs. intramuscular testosterone did not show any significant difference in terms of efficacy for linear growth between the two agents [50]. Lawaetz et al. showed oral T undecanoate formulations were found to be effective in promoting height, inducing secondary sexual characteristics but without affecting bone age advancement [51]. Moreover, a three-month therapy resulted in a significant increase in fat-free mass along with increased height velocity [52]. Transdermal testosterone was found to be effective in promoting growth and virilization in patients with secondary hypogonadism affected by beta-thalassemia [53]. Similarly, 1% testosterone gel was effective in promoting secondary sexual characteristics in boys affected with Klinefelter’s syndrome [54]. Recently, testosterone transdermal gel preparations in strengths of 1% and 2% were found to be safe and effective on adolescent hypogonadal boys with concomitant hypertransaminasemia [55]. Another recent study on boys affected with CDGP has reported equal efficacy of testosterone transdermal gel 2% and intramuscular testosterone in comparison to untreated subjects in increasing height velocity [56]. For patients with partial androgen insensitivity syndrome (PAIS) and 5-alfa reductase deficiency, Dihydrotestosterone gel 2.5% has resulted in increased penile length [57,58]. Furthermore, a randomized, open-label trial on boys with CDGP compared efficacy of intramuscular testosterone (1 mg/kg/4 weeks) to oral letrozole (2.5 mg/day), for promoting puberty, reported a greater rise in gonadotrophins and testicular growth with letrozole although linear growth and bone age advancement did not differ [59]. The testosterone treatment options for the induction of puberty in boys with CDGP and hypogonadism are presented in Table 4. Testosterone Preparation CDGP Hypogonadism T. Enanthate, Cypionate or a mixture of T. esters, IM injections Starting dose: 50 mg monthly, for 3-6 months [46,60] Starting dose: 25-50mg monthly. Increase by 50 mg every 6-12 months [46,60] May increase the dosage by 25-50 mg. Maximum Dose 100 mg [46,60] Adult dosage: 150-200 mg every 2weeks [61] T. Undecanoate IM Injection No data available For puberty induction, only in young men [62] Adult dosage: 750-1000 mg every 10-14weeks [61,62] T. Transdermal gels 10 mg daily for 3 months [56] Gel 1%: 0.5 g/day, increased up to 5 g/day as needed [54]. Adult dosage: 5-10 g/day [61] Gel 2%: Initial dose 10 mg/day [55]. Adult dosage: 40-70 mg/day [61] T. Undecanoate Oral tablets Initial dose 40 mg daily, Maximum dose 80 mg twice daily [51] Adolescent Population: No data 40 mg daily for 4 weeks [50] 40 mg daily for 3 months [52] Adult with hypogonadism , maximum dose is 80 mg twice daily [51] 20 mg daily for 6 months [63] 40 mg daily for mean of 3.5 months [64] T. Transdermal patches Age 12.5 to 15 years: 5 mg over 8-12 hours for 8 weeks [65] Pre-pubertal 14-16 years: 2.5 mg over 12 hours overnight [65] Partially virilized 17-19 years: 2.5 mg daily [65] Virilized men above 20 years: 5 mg daily [53] T. Pellets Subcutaneous No Data Available 13.9 to 17.5 years: 8-10 mg/Kg every 6 months for three doses [53] T. Nasal gel No Data Available No Data Available for the adolescent population T. Transbuccal Bio-adhesive tablet No Data Available No Data Available for the adolescent population Table 4: Summary of the studies done in puberty induction. Monitoring of Testosterone Therapy in Boys Testosterone therapy should be increased gradually to mimic normal pubertal physiology and can be stopped once the HPG axis has been significantly activated, as indicated by an increase in the testicular volume of 6 to 8 mL. Adolescents with permanent hypogonadism, on the other hand, require gradual increases in testosterone dose over two to three years until adult doses are reached to allow for optimal growth [45]. For evaluation of the effectiveness of testosterone therapy in clinical practice, regular follow-up every three to six months is needed along with an assessment of progression of pubertal maturation, height velocity, and changes in body composition [46]. Along with clinical assessment, other imaging, and laboratory workups such as bone mineral density assessment by DXA and hand-wrist radiograph for bone age are useful monitoring tools for both therapeutic benefits and side effects of testosterone therapy. Monitoring is highly recommended and has been standardized for testosterone therapy in hypogonadal men in the recent guideline [61], but such clear guidance is lacking for adolescents [46,66] and studies have shown that these adolescents on testosterone therapy undergo insufficient and incomplete biochemical monitoring [67]. Such wide variations in monitoring can be explained based on many diverse conditions and clinical indications in adolescents necessitating testosterone therapy. It is to be acknowledged that guidelines for clinical and hormonal monitoring for patients undergoing testosterone therapy and targeted approaches based on the etiology of hypogonadism are lacking due to the paucity of studies. With the availability of various newer testosterone formulations and the increasing knowledge of its therapeutic effects, careful monitoring and structured guidelines are needed more than ever. In this regard, Stancampiano et al. proposed a practical approach in a recent article [68]. Based on the temporary or permanent need for ongoing testosterone therapy, they proposed two different schemes for monitoring of replacement therapy and recommended complete blood count, liver function tests, bone age assessment with full clinical evaluation before starting testosterone therapy. This will provide us with not only a baseline, but also the ability to identify underlying diseases such as polycythemia or hypertransaminasemia when testosterone therapy is contraindicated. It will also alert the physician to additional diagnostic work-up for an underlying condition and the selection of preparations with a lower side effect profile, paving the way for individualized monitoring for each patient. Boys with CDGP usually have induction of puberty with a six-month course of testosterone therapy and once the therapy is initiated, full clinical evaluation alone at three- and six-month intervals is usually sufficient. Patients with a strong suspicion of CDGP but who are requiring therapy for more than six months need to be managed differently. They will need thorough evaluation for the underlying etiology and are likely to do better with the monitoring protocol for patients with hypogonadism which includes assessment of bone mineral density along with the metabolic and gonadal profile. Monitoring in cases with permanent hypogonadism requires the bone mineral density assessment by DXA scan using validated methods with adjustment for age, size, and sex along with bone age assessment and serum lipid profile at baseline, one year, and then every one to two years. Thorough clinical evaluation and laboratory assessment such as serum total testosterone and complete blood counts needs to be done at baseline and at three, six, and 12 months followed by periodic assessment every 6-12 months has been suggested while liver function tests and serum level of FSH and LH is to be obtained at baseline [67-69]. The psychosocial impact can be assessed with a standardized QoL tool such as the EQ-5D-Y [70]. The assessment of the effectiveness of testosterone therapy in clinical practice should be based mainly on the clinical response observed such as tanner stage progression (increase in stretched penile length) and development of secondary sexual characteristics (deepening of the voice, muscle mass accretion, facial and body hair growth). However, biochemically, keeping serum total testosterone level in the mid-normal reference range during treatment is much safer for the pubertal stage [46] forming the basis of the recommendation for its laboratory assessment which needs to be done periodically as mentioned above. For testosterone therapy, depending upon the type of preparation used and the timing of its administration, variability is observed in the level of serum testosterone obtained. For intramuscular testosterone enanthate or cypionate, the sample should be collected between the injections, while for testosterone undecanoate, it should be collected before the next dose. The level of testosterone is usually checked two weeks after starting therapy and 3-12 hours after application of transdermal testosterone patch while for transdermal gel preparations, it should be tested two hours after application, two weeks after starting treatment. In case of oral testosterone undecanoate, the level can be checked in a non-fasting state 3-5 hours after ingestion and after at least two weeks of starting therapy. Potential adverse effects of testosterone replacement Adverse effects of testosterone therapy are uncommon in the short-term therapy of three to six months usually indicated for induction of puberty; however, they can occur in those with hypogonadism where long-term therapy is indicated. Erythrocytosis, acne and oily skin, Detection of subclinical prostate cancer, growth of metastatic prostate cancer, and reduced sperm production and fertility are some of the effects for which there is evidence of association with testosterone therapy, while gynecomastia, male pattern balding, growth of breast cancer and induction or worsening of obstructive sleep apnea are few of the uncommon adverse events having weak evidence of association with testosterone therapy [61]. Gonadotropin The stimulation of testicular growth and spermatogenesis with improvement in potential fertility is an additional benefit of gonadotropin treatment over testosterone treatment [71]. Although it is commonly used to treat infertility in adults with CHH, it can also be used to induce puberty in adolescent males with CHH. On the other hand, for an inpatient with CHH, testosterone therapy alone is not a feasible treatment option for stimulating testicular growth. To induce puberty in adolescent boys with CHH, various treatment protocols have been used, including hCG alone or in combination with FSH. The treatment regimen varies between 1,000-1,500 IU for hCG and 75-150 IU for FSH administered intramuscularly three times per week [72]. The hCG dose is to be titrated based on testosterone levels, whereas the FSH dose is usually adjusted based on clinical signs [72]. In a retrospective study of boys with CHH, treatment with 5,000 in weekly hCG injections and monthly testosterone injections had a comparable virilizing effect but the final testicular volume was significantly greater in patients treated with hCG [73]. Nonetheless, a prospective study including adolescents with delayed puberty, the majority of them with absent puberty, the use of hCG and rFSH led to significant testicular growth and induced spermatogenesis in 91% of patients [74]. Using FSH alone may be considered in adolescents with severe GnRH deficiency where the goal of priming with FSH alone is to stimulate the proliferation of immature Sertoli cells before seminiferous tubule maturation [75,76]. Raivio et al. [77] studied a small group of boys aged 9.9-17.7 years with gonadotropin deficiency who were initially treated with FSH alone (two mo-2.8 years) that induced testis growth and increased circulating inhibin B levels, followed by successful pubertal induction with a combination of hCG and r-hFSH. Furthermore, a randomized controlled study of 18 adolescents GnRH-deficient men (CHH) with prepubertal testes (<4 mL) and no cryptorchidism or prior gonadotropin therapy showed FSH pre-treatment followed by GnRH was successful in inducing testicular growth, normalizing inhibin B levels, and promoting fertility [78]. Pre-treatment with FSH prior to testicular maturation appears to compensate for suboptimal testicular development during late fetal life and mini puberty, and thus may be beneficial for optimizing testicular growth and future fertility in adolescent males. It was previously noted that the initial testis size in men with CHH reflects the degree of gonadotropin deficiency and predicts treatment response [79]. Thus, boys with complete gonadotropin deficiency as determined by initial mean testicular volume < 4 mL require both hCG and FSH to achieve full testicular maturation, whereas boys with partial gonadotropin deficiency with initial mean testicular volume, 7 mL usually require only hCG [80]. Gonadotropin-releasing hormone Throughout puberty, the LH and FSH response increases with the progression of puberty, GnRH stimulates the release of both LH and FSH [81]. Pulsatile GnRH treatment may be an option for patients with CHH who have GnRH deficiency but normal pituitary function. The most physiological approach is to use GnRH infused in a pulsatile fashion, with pulse intervals of 90-120 minutes. I.V. infusion results in the most effective pulsatile stimulation and thus the pulsatile release of gonadotropin, whereas sc administration results in more flattened gonadotropin levels, which can also result in adequate gonadal stimulation [82]. For hypogonadotropic males, GnRH treatment will result in a complete development with testicular growth including spermatogenesis and virilization [83]. For optimal testicular growth and spermatogenesis, the individual dose of GnRH and the time required to achieve maximum effectiveness are variable, ranging from 25-600 ng/kg and requiring a minimum of two years [84]. According to Liu et al. [80], pulsatile sc GnRH therapy for two years in adolescents with the complete form of CHH does not significantly accelerate or enhance testicular growth, hasten the onset of sperm production, or increase sperm output compared to hCG/hMG therapy. Thus, whether pulsatile GnRH administration, a more time-consuming treatment modality, does not offer any practical advantages over conventional hCG/hMG therapy in men with idiopathic HH (IHH), especially given the latter's extremely high fertility rate, remains to be seen [85]. Our suggested approach to patient delayed puberty There has been significant variation in the induction of puberty of adolescent males with central hypogonadism, and there is little agreement on proper treatment. A small number of studies, primarily in those with permanent hypogonadism, support our practice. We used a variety of treatment regimens for pubertal induction and completion, all of which were based on our experience rather than evidence provided by carefully designed studies. After several years of clinical practice, these regimens appear to be largely successful in achieving full virilization. The initial testicular size usually reflects the severity of gonadotropin deficiency and predicts the increase in testicular volume in response to treatment in patients with delayed puberty and hypogonadism, so we use it as a guide for selecting the initial treatment option. We use both hCG and FSH in an adolescent boy with a previous history of absent puberty and small testicular size. Although hCG alone can increase testicular volume, combined treatment with hCG and FSH have been shown to result in a better response in terms of final testicular size, because normal levels of both gonadotropins appear to be necessary for appropriate spermatogenesis induction during puberty. If the patient's pubertal development occurs spontaneously and the testicular size is greater than 4 mL, hCG can be started as a monotherapy. When a patient lacks pubertal development and has a testicular size of fewer than 4 mL, the optimal treatment regimen to optimize testicular growth and maximize the potentiality for fertility is unknown; however, we usually begin with FSH as monotherapy; hCG can be added if the patient achieves better testicular growth. Subsequently, we switch to testosterone in both groups when the testicular volume reaches the normal adult range or no further increase in testicular size was obtained. Figure 3 summarized the treatment approach for patients with delayed puberty due to HH (complete or stalled puberty). Figure 3: Suggested treatment approach for patients with delayed puberty due to HH (complete or stalled puberty). However, the treatment is usually easier for older boys with delayed puberty and adult testicular size. Expectant observation or low-dose testosterone therapy are the two treatment options for CDGP patients. Figure 4 summarized the treatment approach for patients with delayed puberty due to CDGP. For patients with delayed puberty due to hypergonadotropic hypogonadism, our approach is to start testosterone at the age of 11-12 years old and gradually increase. Figure 5 summarized the treatment approach for patients with delayed puberty due to hypergonadotropic hypogonadism. Figure 4: Suggested treatment approach for patients with delayed puberty due to CDGP. CDGP - Constitutional delay of growth and puberty
So you have finished reading the how to restart puberty in males topic article, if you find this article useful, please share it. Thank you very much. See more: vitamins to restart puberty, inducing puberty in males, how to induce puberty, smad3, Second growth spurt, restarting biological growth, second puberty in 20s male, Puberty

